Science Platforms Leverage Research to Cure Heart Attacks
Outcome/Accomplishment
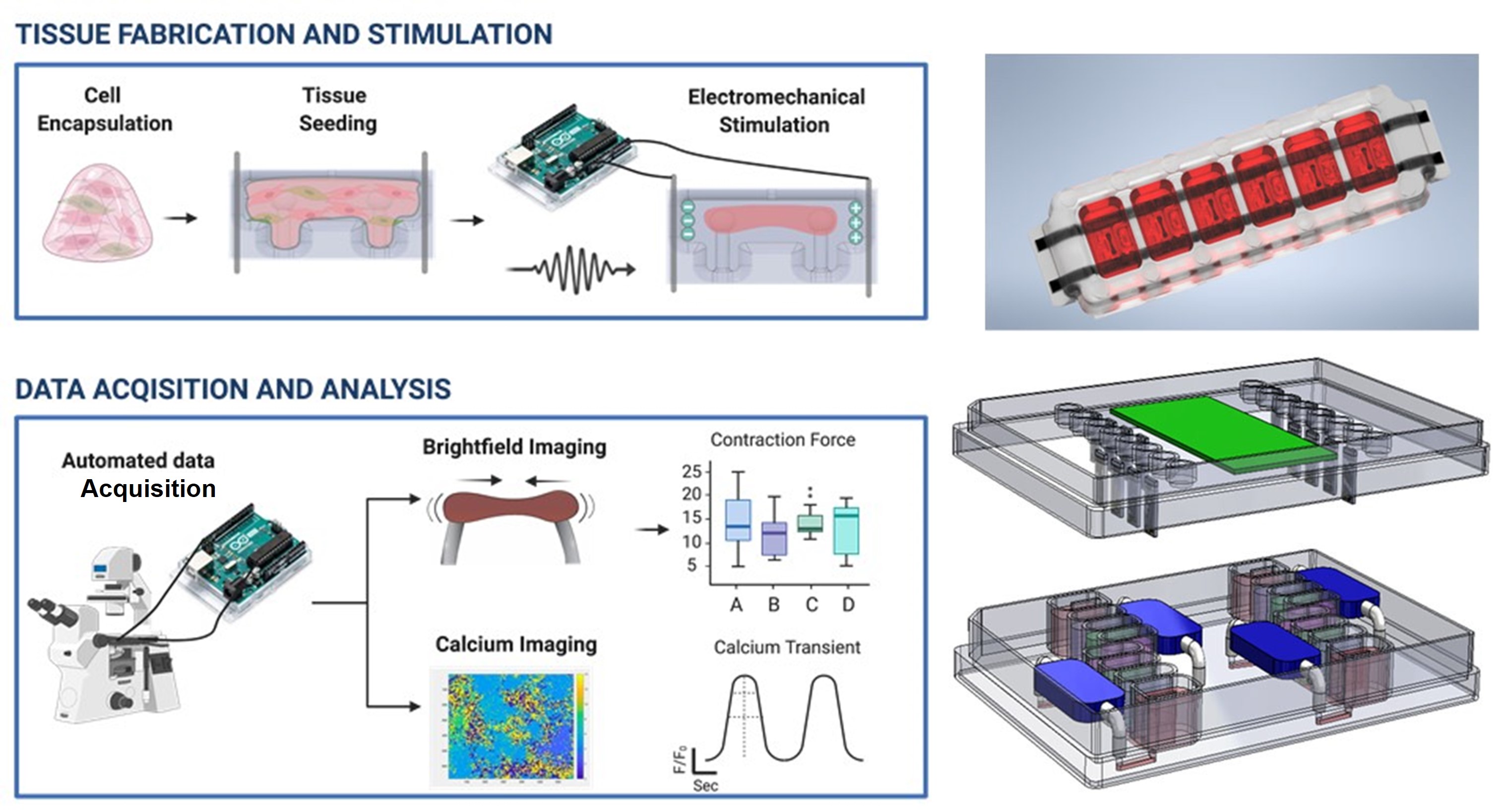
Science platforms are infrastructure developed and used by researchers to increase capacity and opportunity in research, accelerating knowledge diversification, information-sharing, and collaboration among diverse disciplines. A team of university researchers working on a wide-ranging effort to tackle the top killer worldwide—heart attacks—has developed platforms for engineering and producing human cardiac tissue that can be used in life-saving cardiac tissue engineering studies. This research is being supported by the National Science Foundation (NSF)-funded Engineering Research Center (ERC) in Cellular Metamaterials (CELL-MET), headquartered at Boston University (BU).
Impact/Benefits
A heart attack occurs when blood flow to the heart is severely reduced or blocked, usually due to a buildup of fat, cholesterol, and other substances in the heart (coronary) arteries. "Once it's damaged, heart tissue is basically gone forever. You're just going to have to make do for the rest of your life with the healthy tissue that remains," says David Bishop, a materials scientist at BU College of Engineering and director of CELL-MET. Bishop and his colleagues are working on a novel way to reverse heart disease while avoiding the downside of adverse reactions when foreign tissue is used for repairs. Employing the science platforms CELL-MET has developed, they are working to create implantable heart patches using a patient's own skin cells as a starting point. Because they originated from parts of the patient's own body, there is almost no chance that the newly formed cells will trigger an immune response.
Explanation/Background
Science platforms confer advantages in research through increased scientific opportunity, standardization of best practices, and economies of scale. For CELL-MET, these new platforms enable more and better research efforts on implantable heart patches. The heart functions as a highly organized physiological pump. Heart cells are mechanically active—they need to contract and generate force as they grow. Through a complex biological process, the group can reprogram the patient's own skin cells, turning them into pluripotent stem cells—a sort of universal cell that can become almost any kind of tissue in the body. From there, the researchers can slowly coax the cells into becoming cardiomyocytes, the pulsating muscle cells that do the bulk of the heart's work. With the right materials and structure to support them, the cells can more easily mature, align themselves into strings of muscle, and start beating in unison.
Location
Boston, MassachusettsStart Year
Biotechnology and Healthcare
Biotechnology and Healthcare
Lead Institution
Core Partners
Fact Sheet
Outcome/Accomplishment
Science platforms are infrastructure developed and used by researchers to increase capacity and opportunity in research, accelerating knowledge diversification, information-sharing, and collaboration among diverse disciplines. A team of university researchers working on a wide-ranging effort to tackle the top killer worldwide—heart attacks—has developed platforms for engineering and producing human cardiac tissue that can be used in life-saving cardiac tissue engineering studies. This research is being supported by the National Science Foundation (NSF)-funded Engineering Research Center (ERC) in Cellular Metamaterials (CELL-MET), headquartered at Boston University (BU).
Location
Boston, MassachusettsStart Year
Biotechnology and Healthcare
Biotechnology and Healthcare
Lead Institution
Core Partners
Fact Sheet
Impact/benefits
A heart attack occurs when blood flow to the heart is severely reduced or blocked, usually due to a buildup of fat, cholesterol, and other substances in the heart (coronary) arteries. "Once it's damaged, heart tissue is basically gone forever. You're just going to have to make do for the rest of your life with the healthy tissue that remains," says David Bishop, a materials scientist at BU College of Engineering and director of CELL-MET. Bishop and his colleagues are working on a novel way to reverse heart disease while avoiding the downside of adverse reactions when foreign tissue is used for repairs. Employing the science platforms CELL-MET has developed, they are working to create implantable heart patches using a patient's own skin cells as a starting point. Because they originated from parts of the patient's own body, there is almost no chance that the newly formed cells will trigger an immune response.
Explanation/Background
Science platforms confer advantages in research through increased scientific opportunity, standardization of best practices, and economies of scale. For CELL-MET, these new platforms enable more and better research efforts on implantable heart patches. The heart functions as a highly organized physiological pump. Heart cells are mechanically active—they need to contract and generate force as they grow. Through a complex biological process, the group can reprogram the patient's own skin cells, turning them into pluripotent stem cells—a sort of universal cell that can become almost any kind of tissue in the body. From there, the researchers can slowly coax the cells into becoming cardiomyocytes, the pulsating muscle cells that do the bulk of the heart's work. With the right materials and structure to support them, the cells can more easily mature, align themselves into strings of muscle, and start beating in unison.